Several types of antispasmodic treatments are available over the counter (OTC). They include:
- Hyoscine N-butylbromide main ingredient in Buscopan®
- Drotaverine
- Peppermint Oil
Hyoscine N-butylbromide has been a trusted ally in the fight against abdominal cramps for 70 years. The makers of Hyoscine N-butylbromide (Buscopan®) know that for some people, the abdominal pain and cramps won’t relent without a bit of help from an additional painkiller — paracetamol. So, Hyoscine N butylbromide + Paracetamol, a power combo for stronger abdominal pain and cramps, is available in 2 versions:
- Hyoscine N-butylbromide Buscopan®
- Hyoscine N-butylbromide + Paracetamol (Buscopan Venus) Hyoscine N-butylbromide Paracetamol (Buscopan® Plus)
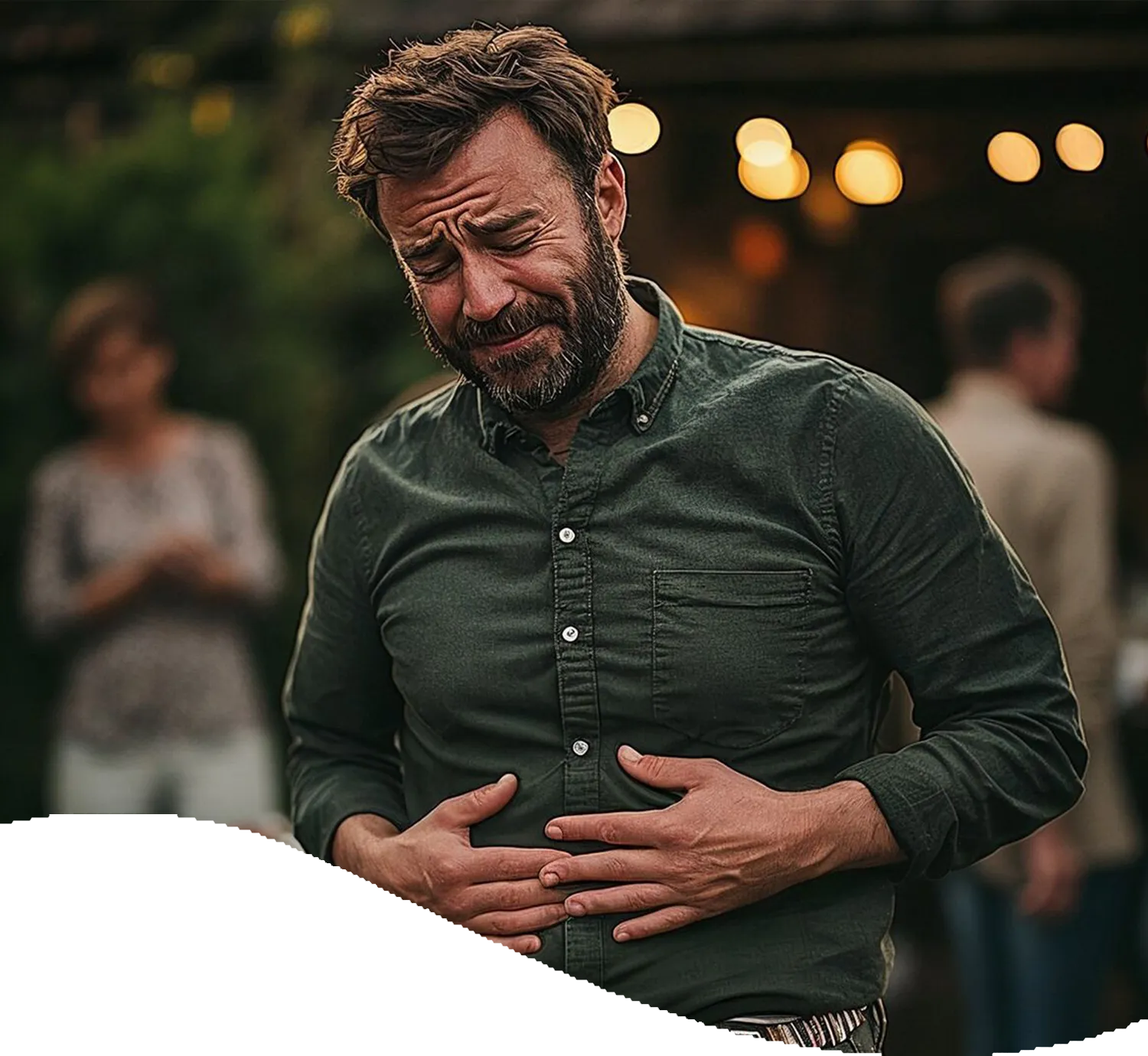
It’s important to note that painkillers, alone or analgesics, are not equally suitable for treating FACP. This is due to a number of reasons.
Firstly, analgesics don’t treat the root cause of the stomach pain, they just block the pain perception and pain signals from the central nervous system. Meanwhile, antispasmodics like Hyoscine N-butylbromide (Buscopan®) act directly on the cause of the pain, and only where needed, by relaxing the contracting muscles in the gut.
Secondly, analgesics or painkillers may also cause some gastrointestinal side effects. Hyoscine N-butylbromide (Buscopan®), on the other hand, is tough on pain, but gentle on the belly. It also works locally on the gut.
Read our article about the difference between antispasmodics and painkillers to learn when to use each.


.webp 0w)
.webp 0w)



.webp)


.webp)






